Why “Eat Less and Move More” Isn’t the Whole Answer to Weight Loss
For decades, weight loss advice has been reduced to a simple equation: eat less and move more. If you’ve ever left a primary care appointment hearing those exact words — with little explanation or support — you’re not alone.
For many people, this advice feels frustrating, dismissive, and ineffective. And if it hasn’t worked for you, it’s not because you lack discipline or motivation. It’s because weight loss is far more complex than calorie math.
At our Dallas-based medical wellness practice, we see this every day: intelligent, motivated individuals doing “everything right” and still struggling with weight, energy, and metabolic health.
Weight Loss Is Not Just About Calories
Your body is not a calculator. It is a highly adaptive biological system regulated by hormones, nervous system signals, metabolism, and environmental inputs.
Calories matter — but they are only one variable in a much larger equation.
Factors that significantly influence weight and fat loss include:
- Hormone balance (insulin, cortisol, thyroid, estrogen, testosterone)
- Blood sugar regulation
- Sleep quality
- Stress and nervous system load
- Gut health and inflammation
- Genetics and metabolic adaptation
When these systems are out of balance, simply eating less and exercising more can actually backfire, leading to plateaus, fatigue, increased cravings, or weight regain.
What Primary Care Often Misses in Weight Loss Care
Primary care providers are skilled at managing acute illness and chronic disease, but weight and metabolic health require time, data, and specialized evaluation that many settings simply don’t allow.
What’s often missing:
- A deeper look at insulin resistance and fasting insulin
- Evaluation of cortisol and stress physiology
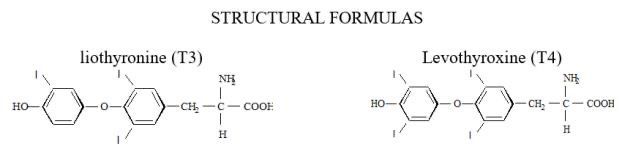
- Assessment of thyroid function beyond basic TSH
- Insight into hormonal drivers of hunger and satiety
- Support for the mental and emotional load of weight management
Most patients receive general advice, a handout, and little follow-up — not personalized metabolic care.
Why the “Eat Less, Move More” Model Fails So Many People
When calorie restriction is applied without addressing root causes, the body adapts defensively.
Common physiological barriers include:
Blood Sugar Dysregulation
Fluctuating glucose levels drive intense hunger, cravings, and energy crashes, making consistency nearly impossible.
Leptin Resistance
Leptin is the hormone that tells your brain you’re full. When resistance develops, satiety signals are blunted — even when enough food is consumed.
Cortisol Overload
Chronic stress elevates cortisol, which promotes fat storage (especially abdominal fat) and disrupts insulin sensitivity.
Thyroid Dysfunction
Low or suboptimal thyroid function slows metabolism, reduces energy expenditure, and makes fat loss more difficult.
This is not a willpower problem.
It’s a systems problem.
A Better Approach: Medical, Data-Driven, and Personalized
At our Dallas medical wellness clinic, we use a functional, evidence-based approach to weight and metabolic health that focuses on why the body is resisting change — not blaming the patient.
Our approach may include:
Comprehensive Lab Testing
We assess markers related to:
- Insulin resistance and glucose regulation
- Thyroid function
- Sex hormones
- Inflammation
- Nutrient status
GLP-1 Therapy (When Appropriate)
Medications such as semaglutide or tirzepatide may be used under medical supervision to support:
- Appetite regulation
- Satiety signaling
- Insulin sensitivity
These therapies are tools — not shortcuts — and are most effective when paired with education and monitoring.
Continuous Glucose Monitoring (CGMs)
CGMs provide real-time insight into how your body responds to food, stress, and sleep — allowing for highly personalized adjustments.
Nutrition Guidance That Supports Physiology
We focus on:
- Adequate protein intake
- Fiber for gut and blood sugar support
- Sustainable habits that reduce food noise
Ongoing Medical Support
Weight loss is dynamic. We monitor progress, adjust plans, and address barriers as your metabolism adapts.
Why Personalized Metabolic Care Matters
Generic advice ignores individuality.
Two people can eat the same calories and exercise the same way — and have completely different outcomes. Personalized care respects that biology, hormones, and lifestyle all matter.
Our patients aren’t handed vague instructions and sent home. They’re supported with structure, data, and medical oversight that evolves over time.
You Deserve More Than One-Size-Fits-All Advice
If you’ve been told to “just try harder” and felt discouraged by lack of results, it may be time for a different strategy.
A smarter approach uses:
- Data instead of guesswork
- Medical insight instead of blame
- Support instead of shame
If you’re in Dallas, TX and looking for a comprehensive approach to weight and metabolic health, our team is here to help.
👉 Book a consultation and let’s build a plan that works with your body — not against it.