Cholesterol & Hormones: Why Your Labs Deserve a Deeper Look Before Statins
Dallas–Fort Worth Hormone Care Perspective
If you’ve been told your cholesterol is “high” and immediately advised to start a statin, you’re not alone.
I see this every week in my Dallas–Fort Worth practice, especially in women navigating perimenopause and menopause. Labs change, symptoms show up, and instead of asking why, the conversation jumps straight to medication.
Cholesterol isn’t just a number to suppress. It’s a foundational molecule your body relies on for hormone production, cellular health, and metabolic balance. When it’s elevated, it often tells a story worth listening to.
Cholesterol Is the Starting Point for Your Hormones
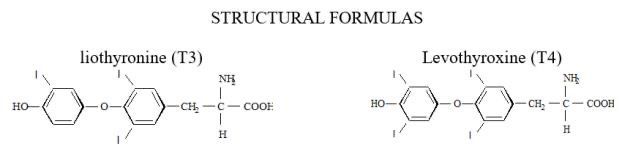
Cholesterol is the building block your body uses to produce all steroid hormones, including estrogen, progesterone, testosterone, cortisol, and even vitamin D.
I often explain it to patients like this: cholesterol is the raw material. Hormones are the finished product. If your body is struggling to produce hormones efficiently, it may alter how it handles cholesterol.
This becomes especially relevant during hormonal transitions such as perimenopause, menopause, postpartum changes, chronic stress states, or thyroid dysfunction. These are the exact scenarios where many people suddenly see their cholesterol rise despite no major lifestyle changes.
Cholesterol Does More Than Affect Your Heart
Cholesterol plays a role in far more than cardiovascular health.
It’s a structural component of every cell membrane in your body, helping cells communicate and maintain stability. It’s also required for bile acid production, which allows you to digest fats and absorb fat-soluble nutrients. Your brain and nervous system depend on it as well.
Your body doesn’t make cholesterol by accident. When levels rise, it’s often responding to an underlying physiological demand or imbalance.
Why Cholesterol Can Rise Even If You Eat “Healthy”
Diet matters, but it’s rarely the whole explanation.
Some of the most common medical contributors to elevated cholesterol include hypothyroidism, insulin resistance or diabetes, chronic stress with elevated cortisol, kidney disease, liver dysfunction, and hormone-altering medications such as oral contraceptives or steroids.
In women, declining estrogen during perimenopause often changes lipid metabolism. LDL may rise, HDL may fall, and triglycerides can shift even when weight and diet remain stable.
There’s also a bidirectional relationship at play. Elevated cholesterol can interfere with pituitary signaling, affecting thyroid-stimulating hormone and reproductive hormones. That means hormone imbalance can raise cholesterol, and high cholesterol can further disrupt hormone balance.
Why I Don’t Believe in Treating Cholesterol in Isolation
Statins are not inherently bad medications. When clearly indicated, they can be lifesaving.
The problem arises when cholesterol is treated without first identifying secondary causes. If hypothyroidism, cortisol dysregulation, or insulin resistance is driving the lipid abnormality, correcting the root issue may significantly improve cholesterol without lifelong medication.
From a clinical standpoint, starting a statin without appropriate evaluation misses an opportunity to practice real medicine.
Before cholesterol-lowering therapy is initiated, a proper workup should include thyroid testing beyond just TSH, glucose and insulin markers, liver and kidney function, and when appropriate, cortisol and sex hormone evaluation.
Major cardiology and endocrine guidelines support this approach, emphasizing that underlying endocrine disorders affecting lipids should be addressed first.
Do Statins Interfere With Hormone Production?
This is a common concern I hear from patients seeking hormone replacement therapy near Dallas.
The evidence is reassuring. Statins do not significantly impair the body’s ability to produce steroid hormones, even though they reduce cholesterol synthesis.
That said, using a statin without understanding why cholesterol is elevated still means treating a lab value instead of the physiology behind it. My goal is always to make decisions with full context.
The Bigger Picture
Cholesterol is not the enemy. It’s information.
When it’s elevated, it may reflect thyroid dysfunction, hormonal transition, chronic stress, or metabolic imbalance. Ignoring that signal and simply suppressing the number doesn’t always serve the patient long term.
This is why my approach to hormone optimization in the Dallas–Fort Worth area is lab-guided, individualized, and focused on root cause evaluation rather than one-size-fits-all protocols.
Looking for Hormone-Focused Care in Dallas or DFW?
If you’re searching for hormone replacement therapy near you, functional hormone testing in Dallas, or a provider who looks at cholesterol through a hormone-informed lens, you’re in the right place.
I offer comprehensive hormone evaluation and personalized treatment plans for women and men, both in-clinic and via telehealth where licensed.
If you’ve been told your labs are “normal” but you don’t feel normal, or if cholesterol changes showed up without explanation, I’m happy to help you sort through it.
You can request a consultation to review your labs, symptoms, and goals together and decide on the most appropriate next steps.
-Jae
214-890-6180