Weight Loss, Metabolic Health & Hormone Support — Without Punishment
Get You a Health Optimization Plan That Can Do Both
More Than Muscles and Mirrors
When most people think about exercise, they picture a certain body type, a smaller number on the scale, or a “before and after” moment.
But movement was never meant to be about punishment or appearance alone.
Exercise is one of the most powerful tools we have for health optimization — influencing mood, metabolism, hormones, longevity, and safety from the inside out.
At Optimize by JaeNix, we help patients reframe exercise not as something you do to your body, but something you do for your body.
Exercise and Mood: Supporting the Brain, Not Just the Body
Movement has immediate effects on brain chemistry — sometimes within minutes.
Regular exercise has been shown to:
- Support serotonin and dopamine pathways involved in mood regulation
- Increase endorphins, which contribute to feelings of well-being
- Improve sleep quality, a cornerstone of mental and metabolic health
- Help regulate cortisol, supporting the stress response
For some individuals, consistent movement can play a meaningful role alongside other supports for mild mood concerns. This isn’t about extremes — even walking, mobility work, or gentle strength training can make a difference.
Exercise, Metabolism & Weight Support
Weight loss and metabolic health are often treated as calorie math, but the body is more complex than that.
Exercise supports metabolic health by:
- Preserving lean muscle, which influences resting metabolic rate
- Improving insulin sensitivity and blood sugar regulation
- Supporting energy stability and recovery
- Working synergistically with nutrition strategies and, when appropriate, tools like GLP-1 therapy
GLP-1 medications can support appetite regulation and metabolic health, but movement remains essential for preserving muscle, protecting metabolism, and supporting long-term sustainability.
Medication is a tool — movement is a foundation.
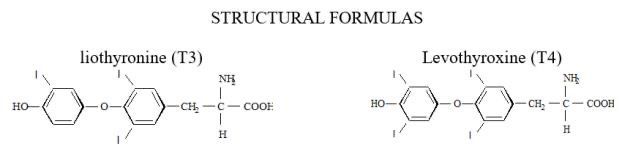
Exercise and Hormone Health
Hormones influence how the body responds to exercise — and exercise influences hormone signaling.
Regular movement can support:
- Insulin and blood sugar balance
- Cortisol regulation
- Estrogen and progesterone metabolism
- Overall resilience during perimenopause and menopause
For individuals using hormone therapy (HRT/BHRT), exercise often complements care by supporting energy, sleep, and metabolic stability. The goal is not intensity for intensity’s sake, but appropriate, sustainable movement that fits your phase of life.
Exercise and Longevity: Adding Life to Your Years
Exercise isn’t just about living longer — it’s about living better.
Consistent physical activity is associated with:
- Reduced risk of cardiometabolic disease
- Improved cognitive health and brain resilience
- Preserved mobility and independence with aging
Strength training in particular plays a key role in maintaining muscle mass, bone density, and balance — all critical factors in long-term health span.
Exercise and Safety: Training for the Future
Movement is protective.
A well-designed exercise plan can:
- Improve balance and coordination
- Reduce fall and fracture risk
- Support joint health and mobility
- Enhance functional strength for daily activities
This becomes increasingly important as we age, when falls and injuries are a major cause of loss of independence.
Rethinking Exercise: From Punishment to Prescription
Exercise was never meant to be about “earning food” or undoing guilt.
At Optimize by JaeNix, we view movement as a prescription for whole-body health — supporting mood, metabolism, hormones, and long-term function.
Whether someone is:
- optimizing metabolic health
- using GLP-1 therapy
- navigating perimenopause or menopause
- or simply rebuilding consistency
We design movement plans that fit real lives, real bodies, and real goals — not trends.
Ready to Build a Plan That Supports It All?
If you’re ready for an exercise strategy that supports your metabolism, hormones, and long-term health — not just your appearance — we’re here to help.
📍 Dallas, TX | Optimize by JaeNix
🔗 Schedule an education-first virtual consultation to get started.