Continuous Glucose Monitoring (CGM) at Optimize by JaeNix
At Optimize by JaeNix, Continuous Glucose Monitoring (CGM) is used as a metabolic optimization tool, not just for diabetes. CGM allows us to see how your body responds to food, stress, sleep, hormones, and medications in real time so we can optimize energy, weight, and metabolic health with intention instead of guesswork.
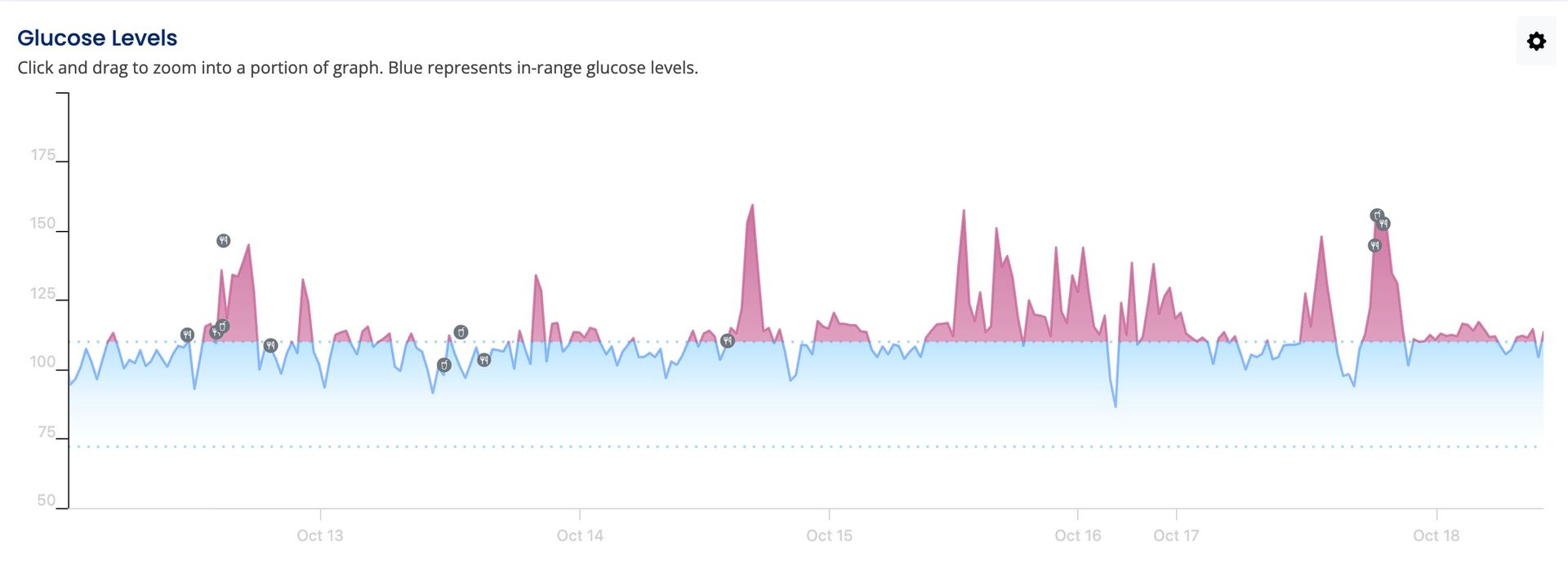
We partner with Theia Health, which gives us a shared dashboard to review your glucose data together. This allows for personalized guidance based on your actual physiology, not generic nutrition plans or one-size-fits-all advice.
Why CGM Matters More Than Most People Realize
Many patients are surprised to learn that you can have “normal” lab results and still experience daily glucose dysregulation.
Common misconceptions include thinking that:
- Normal fasting glucose automatically means good metabolic health
- Glucose only matters if you have diabetes
In reality:
- Glucose instability drives cravings, fatigue, inflammation, poor sleep, and fat storage
- These patterns often show up years before diabetes develops
- The same food can affect you very differently depending on:
- what you eat it with
- time of day
- sleep quality
- stress levels
CGM makes these invisible patterns visible—and actionable.
Why Glucose Is So Important for Long-Term Health
What “Normal” Really Means
Traditional guidelines often define:
- Normal fasting glucose as under 100 mg/dL
- Normal post-meal glucose as under 140 mg/dL
However, research suggests that optimal metabolic health often exists at lower ranges:
- Fasting glucose closer to 72–85 mg/dL
- Post-meal glucose around 115 mg/dL
- Ideally with less than a 30 mg/dL spike after meals
Even glucose values considered “high normal” have been associated with increased risk.
What the Research Shows
- A 3-fold increase in Type 2 diabetes risk when fasting glucose is 91–99 mg/dL compared to levels below 83 mg/dL
- Higher cardiovascular disease risk when fasting glucose is 95–99 mg/dL compared to levels below 80 mg/dL
- Men with fasting glucose above 85 mg/dL have significantly higher cardiovascular mortality than those below 85 mg/dL
These findings help explain why many people struggle with energy, weight, and inflammation long before a formal diagnosis ever appears.
What We Expect to See in Healthy, Non-Diabetic Individuals
Based on multiple clinical studies using CGMs, metabolically healthy individuals often show:
- Average fasting glucose around 85–92 mg/dL
- Over 90% of time spent between 70–140 mg/dL
- Less than 4% of time above 140 mg/dL
- Average post-meal glucose around 121–123 mg/dL
CGM lets us see how closely (or how far) your real life matches these patterns.
What You’ll Learn From CGM
Using CGM with Theia’s platform, you’ll gain insight into:
- How food combinations affect glucose differently than foods eaten alone
- Why the same meal may spike glucose at dinner but not at breakfast
- How meal composition impacts energy and post-meal fatigue
- Your personal glucose patterns, unique to your body
- How much time you spend in an optimal glucose range (often 70–110 mg/dL)
The app includes photo-based meal logging, macro and nutrient breakdowns, and easy-to-read trend visualization—making the data usable, not overwhelming.
How Glucose Directly Impacts Common Health Goals
Energy & Brain Function
Your brain relies heavily on glucose. Both high and low glucose levels can cause fatigue and reduced mental clarity.
- High glucose can lead to the classic post-meal crash
- Low glucose can leave you feeling sluggish, shaky, or foggy
Stability matters more than extremes.
Weight Loss & Fat Storage
Blood glucose and insulin are tightly linked.
- Higher glucose → higher insulin
- Higher insulin → fat storage rather than fat burning
If insulin stays elevated, weight loss becomes an uphill battle regardless of calories or effort.
Mental Clarity
Research shows that people who experience larger glucose spikes and slower recovery perform worse on memory and cognitive testing. CGM helps identify patterns that may be contributing to brain fog or poor focus.
Exercise Performance
Athletes often experience “bonking,” or sudden fatigue from glucose depletion. CGM allows for smarter fueling—helping time carbohydrate intake to prevent crashes and improve performance.
Who Benefits Most From CGM
CGM is especially helpful for patients with:
- Insulin resistance or metabolic dysfunction
- Weight-loss plateaus
- PCOS, perimenopause, or menopause-related changes
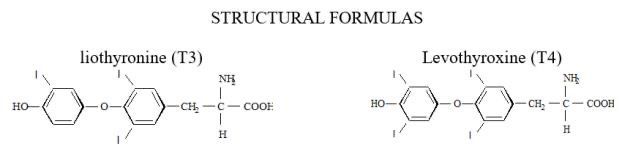
- Thyroid dysfunction
- Fatigue, brain fog, or energy crashes
- GLP-1 therapy optimization
- High stress or irregular schedules
This is precision metabolic care, not calorie counting.
CGM Program Options
Patients may choose one of two pathways depending on how they prefer to obtain sensors.
Option 1: Purchase Sensors Through Theia Health
When sensors are purchased through Theia, there is no monthly platform fee.
Libre Sensors (15-day wear)
- First month: $297
- $99 one-time activation
- $198 for two sensors
- Ongoing: $198/month
- 3-month total: $693
Dexcom G7 Sensors (10-day wear)
- First month: $396
- $99 one-time activation
- $297 for three sensors
- Ongoing: $297/month
- 3-month total: $990
Option 2: Bring Your Own Sensor
Often the most cost-effective option.
- $35/month Theia platform access
- No activation fee
Compatible sensors include Libre 14-day, Libre 2/3 (and Plus versions), and Dexcom G7.
Sensor Cost-Saving Options
When clinically appropriate, I can send a prescription to your pharmacy so you can:
- Attempt insurance coverage (not guaranteed)
- Use manufacturer or pharmacy savings programs
Coverage varies by plan and diagnosis.
For transparency: I personally used CGM and paid $75 for two sensors through my own insurance. This is shared as an example, not a promise.
What’s Included in the CGM Program
Regardless of sensor option:
- Provider-guided CGM use
- Access to the Theia Health dashboard
- Real-time glucose tracking and pattern analysis
- Meal logging with nutrition insights
- Personalized guidance for energy, weight, and metabolic health
- Integration with hormone, GLP-1, thyroid, or peptide care when appropriate
This is guided interpretation, not self-tracking alone.
Important Notes
- CGM for metabolic optimization is not diabetes treatment
- CGM does not replace medical care or lab monitoring
- Insurance coverage is not guaranteed
- Eligibility is determined by provider discretion
Why We Offer CGM at Optimize by JaeNix
Because data changes behavior, and understanding your body changes outcomes. CGM allows us to move beyond calorie counting and into concierge, precision metabolic care that fits real life.
CGM can be added during a consultation or layered into an existing program.
Ready to Get Started or Have Questions?
If you’re interested in adding Continuous Glucose Monitoring (CGM) or want to learn how it fits into one of our hormone, metabolic, peptide, or primary care programs, we’re happy to help.
Optimize by JaeNix / JaeNix, PLLC
📍 Dallas, TX (In-Clinic & Telehealth Options Available)
📞 Call or Text: 214-890-6180
📧 Email: contact@jaenixmedspa.com
Our team can help you:
- Determine if CGM is appropriate for your goals
- Review sensor options and cost-saving pathways
- Schedule a consultation or add CGM to an existing program
- Explore other concierge medical and aesthetic services
Telehealth services are currently available in TX, CO, FL, VT, WA, CT, and IA, with additional states coming soon.
(AR, CA, TN, IN, PA, OK are pending - so watch for those soon!)
We look forward to supporting your next step toward optimized health.
-Jessica, APRN